Limited Long-Term Data Fuels Debate on Puberty Blockers' Impact on Child Fertility and Sexual Function
A recent tweet from @spiked highlighted significant concerns regarding the long-term effects of puberty blockers on children, specifically their potential impact on natural puberty, fertility, and sexual function. The tweet quoted Helen Joyce, stating, "> 'Children who start early on puberty blockers can never experience natural puberty. They will probably never have an orgasm or be fertile. Adults are selling them a fantasy,' on The Brendan O’Neill Show." This statement underscores an ongoing debate among medical professionals, ethicists, and policymakers concerning gender-affirming care for minors.
Puberty blockers, scientifically known as Gonadotropin-Releasing Hormone (GnRH) analogues, are medications used to temporarily halt pubertal development. While initially used for precocious puberty, their application expanded to include adolescents experiencing gender dysphoria, aiming to provide time for identity exploration and prevent the development of unwanted secondary sexual characteristics. However, the long-term implications of these treatments, particularly when initiated in early puberty, remain a subject of extensive discussion due to a scarcity of comprehensive longitudinal studies.
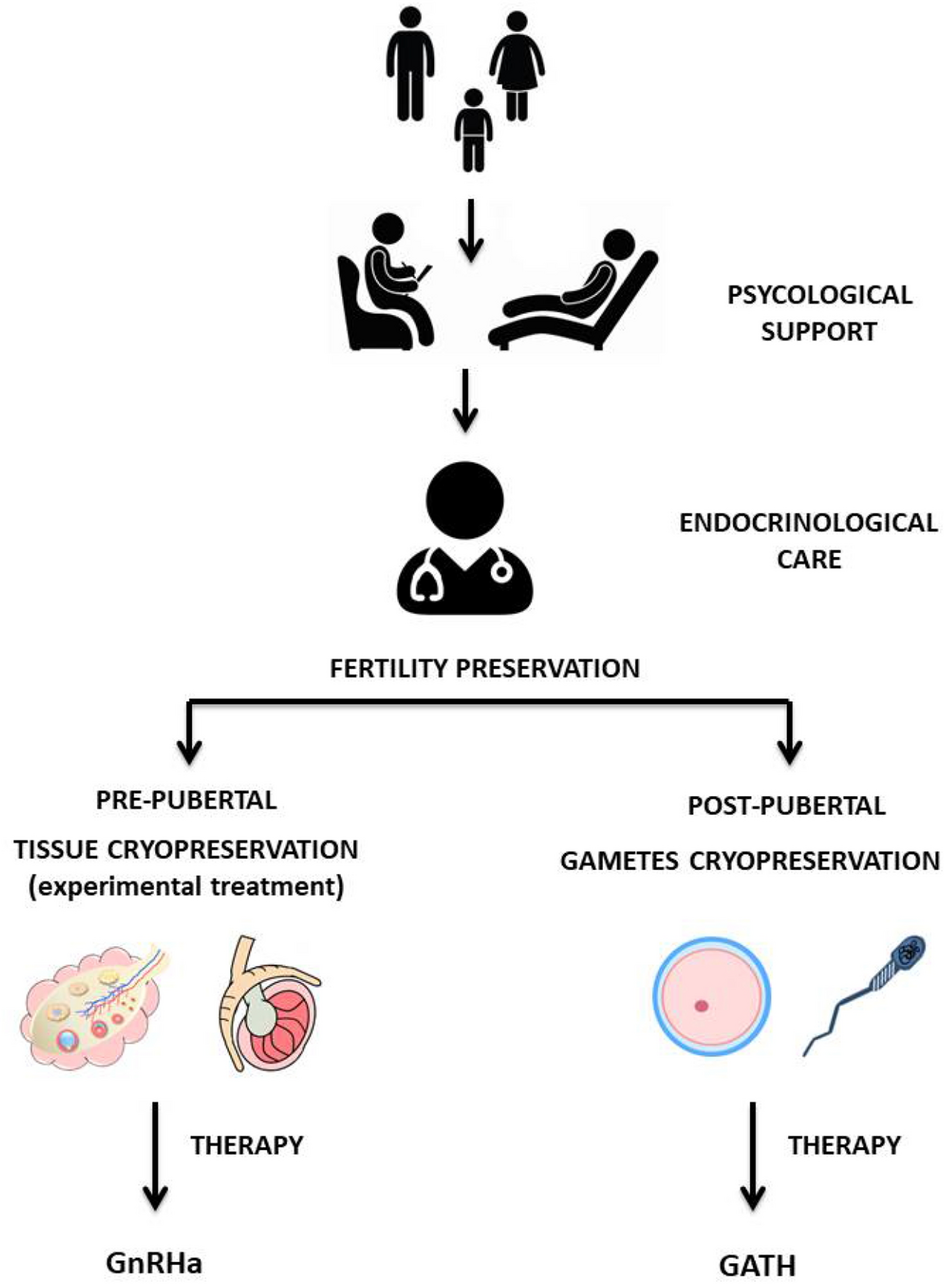
Concerns about fertility are prominent, with research indicating that if puberty blockers are followed by cross-sex hormones, proven methods of fertility preservation are limited, especially for those who initiate treatment before significant pubertal development. Studies suggest that while GnRH analogues themselves may not cause permanent gonadal damage, the subsequent use of cross-sex hormones can impair future reproductive capacity. The ethical principle of a "child's right to an open future" is often invoked, questioning whether minors can provide truly informed consent for treatments with potentially irreversible consequences on fundamental life aspects like reproduction.
Beyond fertility, the impact on sexual function and libido is also under scrutiny. Experts have raised concerns that suppressing puberty, particularly in early stages, followed by cross-sex hormones, might adversely affect orgasm capacity due to a lack of natural genital tissue development. While some studies report no negative effects on sexual function when followed by gender-affirming hormone therapy, others highlight a dearth of research and potential risks to physiological arousal and orgasm, especially with certain surgical outcomes.
The debate extends to other potential side effects, including bone mineral density, brain development, and overall growth patterns, with calls for more rigorous safety and effectiveness evaluations. Regulatory bodies, such as NHS England, have recently ceased routine prescribing of puberty blockers to under-18s outside of clinical research settings, citing insufficient evidence for their safety and clinical effectiveness. This shift, influenced by reviews like the Cass Report, emphasizes the need for robust, long-term studies to fully understand the benefits and potential harms of these interventions.