Nurse Alleges Widespread COVID-19 Death Mislabeling Amid Hospital Financial Incentives
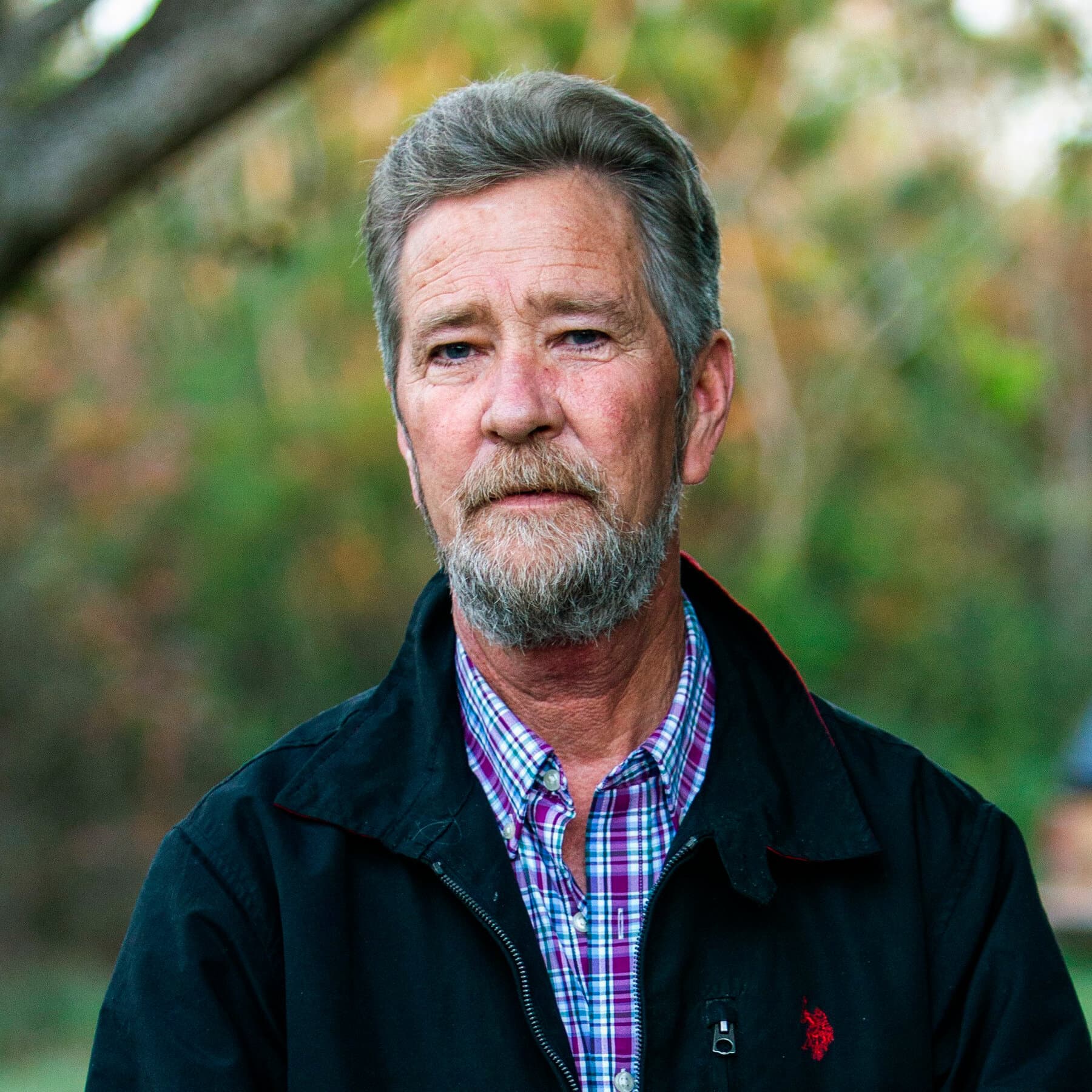
Aformer California nurse, Gail McCrae, has publicly claimed that hospitals, including her former employer Kaiser Permanente Santa Rosa, deliberately mislabeled non-COVID-19 deaths as COVID-19 fatalities, driven by financial incentives. In a recent social media post, McCrae stated, "I observed charts and death records being documented as COVID when they weren't, yes... I have discovered since then there is incentivization going on, there's massive payouts, and that almost definitely plays a role in why we were being told to document these deaths and these admissions as COVID when they weren't." She further characterized the PCR test as "a huge scandal from the get-go."
McCrae, who was reportedly terminated for refusing a COVID-19 vaccine, has been vocal on alternative news platforms, alleging that hospital protocols during the pandemic, such as the use of Remdesivir and patient isolation, contributed to patient deaths, which she termed "medical murder." She also suggested that Electronic Medical Record (EMR) systems were configured to default COVID-19 cases to "unvaccinated" status, potentially skewing data.
During the pandemic, the U.S. government indeed allocated substantial financial assistance to hospitals through the Coronavirus Aid, Relief, and Economic Security (CARES) Act. Studies on the distribution of these funds indicate that higher levels of funding were directed to academic-affiliated hospitals and those reporting a greater number of COVID-19 cases. These funds were intended to cover healthcare-related expenses and compensate for lost revenue due to the public health emergency.
Regarding the accuracy of PCR tests, mainstream scientific consensus generally regards them as the "gold standard" for diagnosing SARS-CoV-2 infection due to their high specificity. However, medical literature acknowledges the potential for false positive results, which can occur due to factors such as laboratory contamination, extremely low viral loads detected at very high cycle threshold (Ct) values, or other technical artifacts. False negatives can also arise from improper sample collection or early-stage infection. Experts emphasize that the interpretation of Ct values requires clinical expertise and cannot be universally applied as a simple cutoff. The psychological and social impact of false positive diagnoses on individuals has also been noted in medical reports.
Official health organizations and hospital associations have largely defended their reporting practices and the integrity of COVID-19 data throughout the pandemic, maintaining that diagnostic and death reporting followed established guidelines. Claims of widespread, deliberate mislabeling for financial gain have been widely refuted by these bodies, though individual cases of data discrepancies or reporting errors may have occurred.