Physician Compensation Debate Intensifies: 70% Deem Relative Value Units Poor Productivity Measures
The system of Relative Value Units (RVUs), a cornerstone of physician compensation in the United States, is facing increasing scrutiny and widespread dissatisfaction among medical professionals. A recent Medscape survey revealed that a significant 70% of physicians consider RVUs to be poor measures of productivity, with 60% expressing unhappiness over their financial impact. This sentiment echoes a pointed critique from "The Rogue Dermatologist," who stated in a recent tweet, > "RVUs are a tool for price controlling and synthetically discounting the labor and expertise of physicians, essentially coercing them all to accept equal pay regardless of their individual value, as well as equating the utility of doctors with that of physician assistants and nurse practitioners."
Introduced in 1992 by the Centers for Medicare and Medicaid Services (CMS) as part of the Resource-Based Relative Value Scale (RBRVS), RVUs were designed to standardize physician reimbursement. They comprise three main components: physician work, practice expense, and professional liability insurance, with physician work RVUs (wRVUs) being the largest factor. The system originated from a 1988 Harvard study aiming to quantify the time, skill, and effort involved in various patient care services, and other payers often use the CMS model as a benchmark.
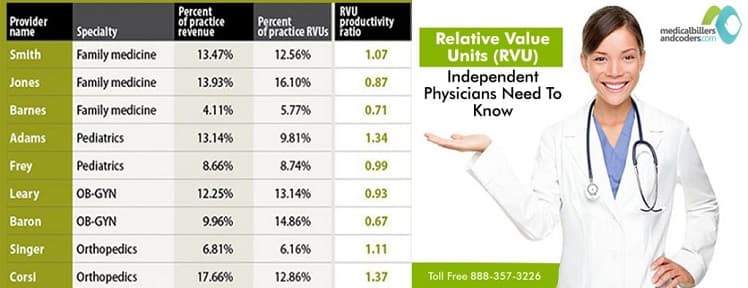
Despite their intended purpose of bringing consistency to healthcare payments, wRVUs have become a primary driver of physician compensation, often serving as a proxy for productivity. The Medscape report further highlighted that 42% of doctors surveyed had their salaries affected by RVUs, with a quarter basing their entire salary on these units. This reliance often pressures physicians to increase patient volume, leading to concerns about rushed encounters and potentially compromising the quality of care.
Critics argue that the RVU system disproportionately rewards procedural interventions over complex cognitive care, such as detailed patient assessments and care coordination. Research in pediatric urology, for instance, suggests the system favors shorter, less complex procedures, failing to adequately compensate for longer, more intricate cases. The American Medical Association's Specialty Society Relative Value Scale Update Committee (RUC), which recommends RVU values to CMS, has been criticized for historically over-valuing physical procedures and under-valuing cognitive services. Furthermore, CMS's budget neutrality mandate means that increasing reimbursement for one service often necessitates decreasing it for another, intensifying competition among specialties.
The perceived disconnect between RVU-based pricing and patient utility is not limited to the U.S., with a South Korean study finding a negative correlation between RVUs and Quality-Adjusted Life Years (QALYs), particularly for procedures with higher fatality potential. This growing discontent is pushing discussions towards alternative payment models that prioritize value over volume. Recent regulatory changes, such as the HHS's finalization of new protections under the Stark Law for value-based arrangements, signal a governmental push towards compensation structures that emphasize coordinated, high-quality care rather than just the quantity of services provided.