COVID mRNA Vaccines Double 3-Year Survival for Cancer Patients on Immunotherapy
New research presented at the 2025 European Society for Medical Oncology (ESMO) Congress reveals that receiving a SARS-CoV-2 mRNA vaccine significantly improves survival for patients with non-small cell lung cancer (NSCLC) and melanoma undergoing immune checkpoint inhibitor (ICI) therapy. Patients who received an mRNA COVID vaccine within 100 days of starting ICI treatment were found to be twice as likely to be alive three years after therapy compared to unvaccinated individuals. This groundbreaking finding, also published in Nature, suggests a potent off-target effect of the vaccines in cancer treatment.
The study, led by researchers at The University of Texas MD Anderson Cancer Center and the University of Florida, analyzed data from over 1,000 patients. For those with advanced NSCLC, vaccinated patients had a median survival of 37.33 months, significantly higher than the 20.6 months for unvaccinated patients. In metastatic melanoma patients, the median survival for vaccinated individuals had not yet been reached, compared to 26.67 months for the unvaccinated group, indicating a substantial improvement.
The mechanism behind this synergy involves the vaccine triggering a strong type I interferon surge, which acts as an "alarm" for the immune system. This surge activates antigen-presenting cells and primes T cells, enhancing adaptive immunity against cancer. As stated in the tweet by Stephen Pimentel, "The vaccine triggers a strong type I interferon surge that activates antigen-presenting cells, primes T cells, and enhances adaptive immunity, while ICIs sustain these T cell responses and counter tumor-induced PD-L1 upregulation."
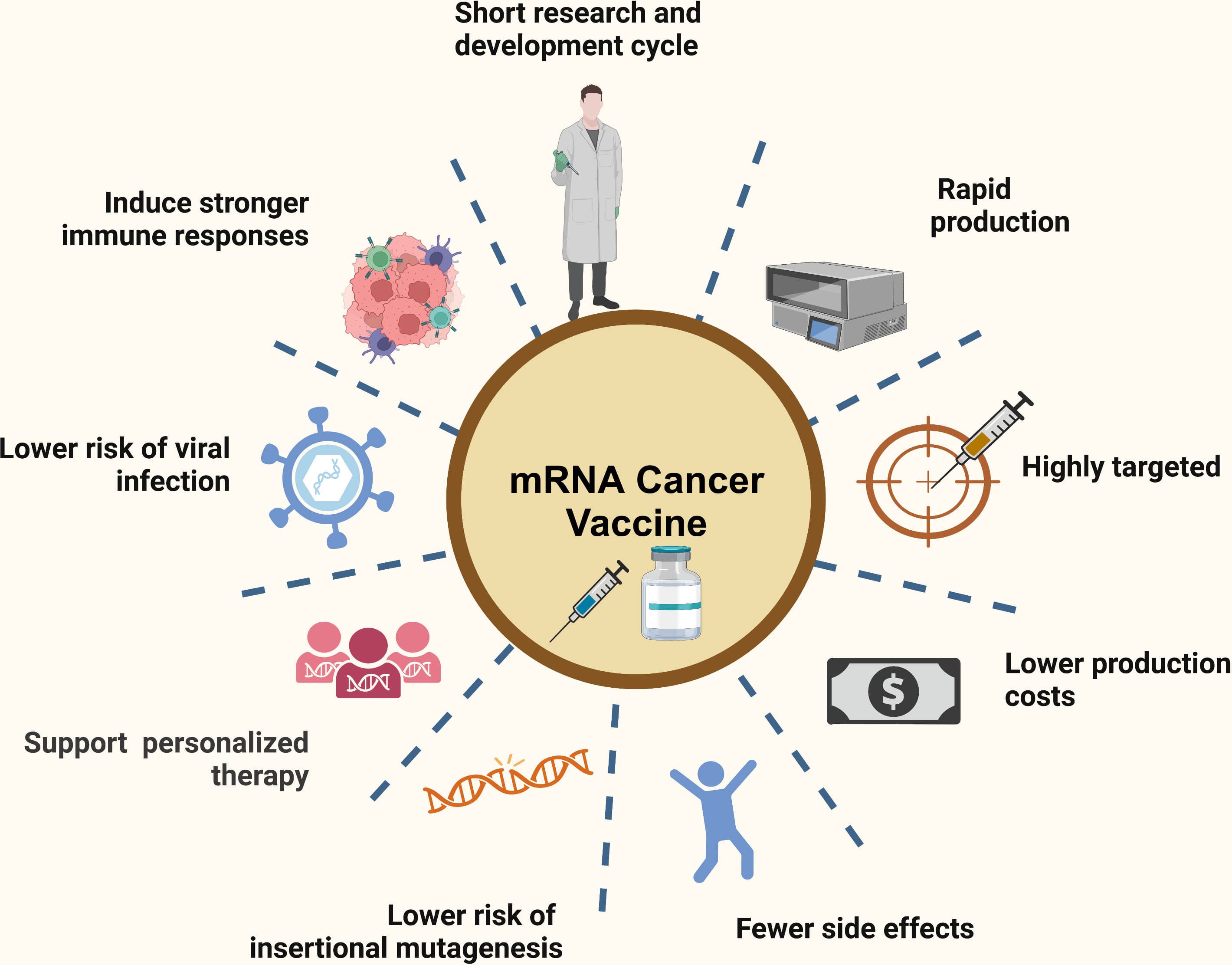
This immune reprogramming sensitizes otherwise unresponsive "cold" tumors by increasing their PD-L1 expression, making them susceptible to ICI therapy. Dr. Adam Grippin, a senior resident in Radiation Oncology involved in the study, noted that commercially available mRNA COVID vaccines "can train patients’ immune systems to eliminate cancer." A multi-center, randomized Phase III trial is currently being designed to further validate these findings and explore the integration of mRNA COVID vaccines into standard cancer care.