71% of Weight Loss Studies Overrepresent Women, Raising Questions on Generalizability
Research in weight loss interventions consistently features a significant gender imbalance, with women overwhelmingly represented while men remain a distinct minority. According to Dr. Chris Masterjohn, a prominent figure in nutritional sciences, this disparity is stark: > "False. Women are grossly overrepresented in weight loss studies. Men are grossly underrepresented. 71% of studies have more women than men. Men are 23% of study participants." This observation, supported by a 2015 systematic review, continues to be reflected in recent research, prompting discussions about the generalizability and efficacy of current weight management strategies.
The statistics cited by Masterjohn originate from a systematic review published in Obesity Reviews (PMID 25494712), which found that 71% of weight loss studies included more women than men, with men constituting, on average, only 23% of participants. This trend persists in contemporary research. For instance, a 2025 study on severe obesity treatment in Brazil reported that women comprised 70% of their hospitalized patient cohort, while a Polish study on real-world weight management programs in Endokrynologia Polska (2025) noted an almost identical distribution of 78% women and 22% men.
This consistent underrepresentation of men in weight loss research raises questions about the applicability of findings across genders. Some studies, such as a 2025 report in PLOS ONE, indicate that men may experience more pronounced fat mass reduction and better preservation of skeletal muscle mass during weight loss interventions compared to women. Conversely, the 2025 Endokrynologia Polska study found no significant gender differences in overall weight reduction, and the original 2015 systematic review concluded there was "little evidence" to suggest men and women require different weight loss strategies, despite the participant imbalance.
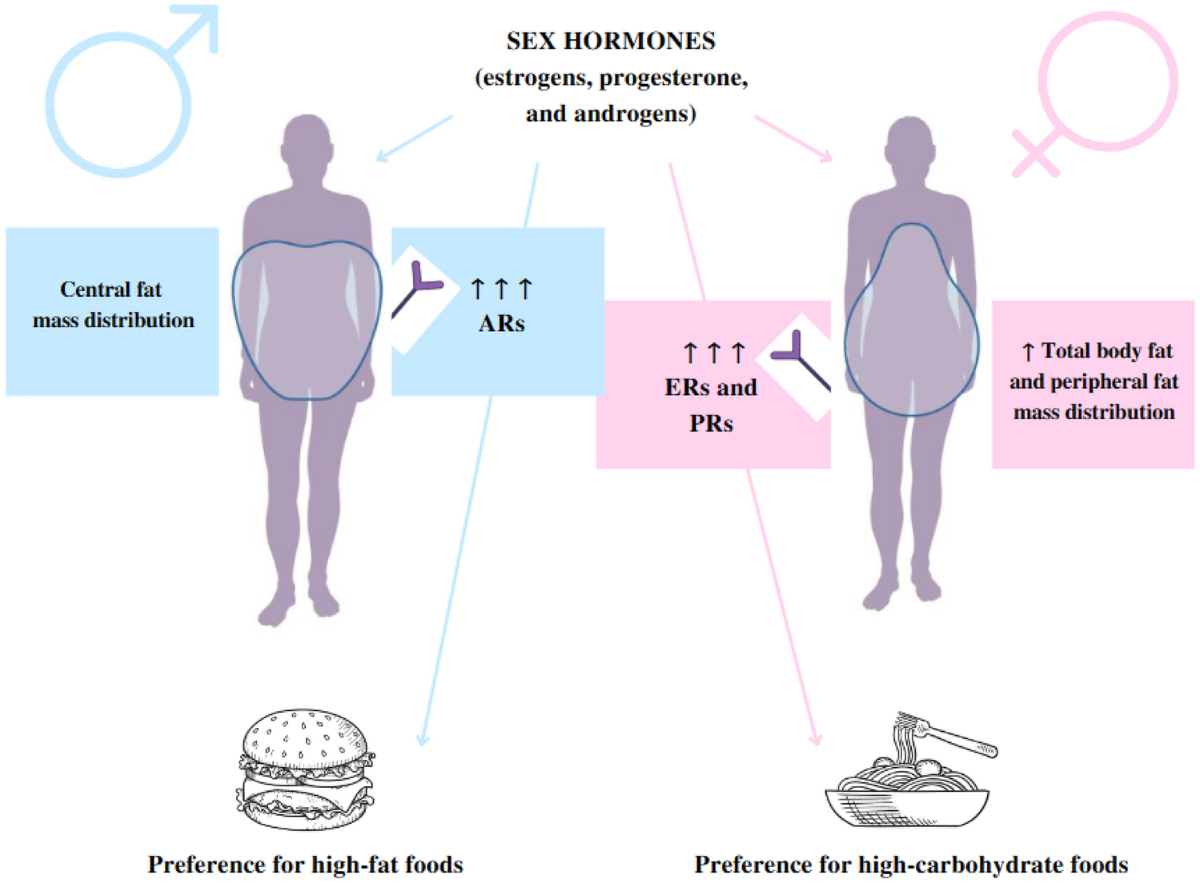
The disparity in study populations can be attributed to factors like inherent metabolic differences, as men typically have higher muscle mass and resting energy expenditure, and varying health-seeking behaviors between genders. The prevalence of female-dominated cohorts limits the generalizability of research outcomes, potentially hindering the development of optimally tailored weight management approaches for men. Addressing this persistent imbalance is crucial for a more comprehensive understanding of weight loss mechanisms and for creating effective, inclusive interventions for all individuals.