Orthorexia: The Dark Side of Healthy Eating, Leading to Fragility and Obsession
A recent social media post by AJAC has highlighted a growing concern: the potential for increased health knowledge to foster an "orthorexic mindset," characterized by "obsession, paranoia, [and] hypochondriac reactivity." The tweet warns that if a "health journey is making you more mentally and physically fragile, you're going down the wrong path." This statement underscores the often-overlooked negative psychological impacts of an extreme focus on "healthy" eating.
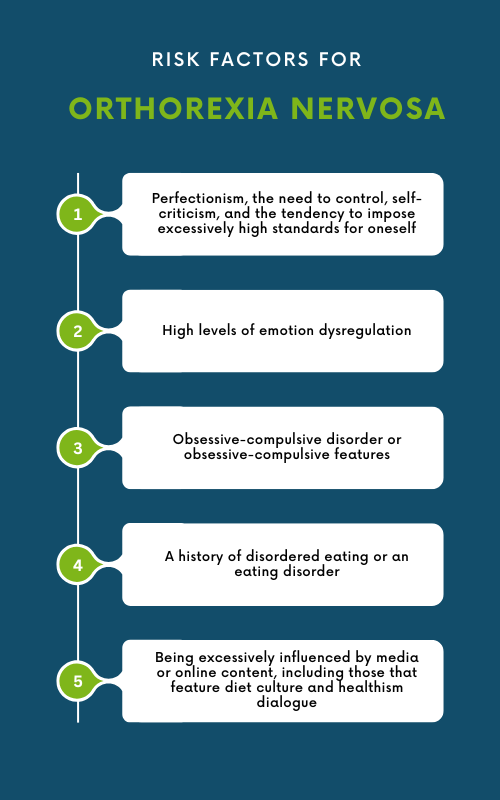
Orthorexia nervosa, a term coined by Dr. Steven Bratman in 1996, describes an unhealthy fixation on consuming only "pure" or "healthy" foods. While not yet an official diagnosis in the DSM-5, it is increasingly recognized by medical professionals as a form of disordered eating. Individuals with orthorexia often develop rigid dietary rules, avoiding entire food groups out of fear that they are not "clean" enough, and may spend excessive hours researching food and planning meals, leading to significant distress and impairment.
Medical experts note similarities between orthorexia and other eating disorders like bulimia and anorexia nervosa, particularly in the element of control over food. However, orthorexia primarily centers on the perceived quality and purity of food rather than quantity or body image concerns. This intense preoccupation can lead to social isolation, as individuals may avoid eating food prepared by others or decline social engagements where their strict dietary standards cannot be met.
The consequences of orthorexia extend beyond mental distress, potentially leading to physical health issues. Restrictive diets can result in nutritional deficiencies, severe weight loss not intended for aesthetic reasons, and other medical problems. Recent research, such as a 2025 study in the Journal of Eating Disorders, suggests that adolescents with chronic conditions requiring strict diets, like celiac disease, show a higher tendency towards orthorexia and impaired eating attitudes. This indicates that while the initial intent is health-driven, the extreme application can paradoxically harm overall well-being.
Treatment approaches for orthorexia often involve a multidisciplinary strategy including psychoeducation, cognitive-behavioral therapy (CBT), and nutritional counseling. These interventions aim to challenge rigid beliefs about food, foster a more balanced and flexible approach to eating, and address underlying psychological factors. The goal is to help individuals develop a healthier relationship with food and regain mental and physical resilience.