Steve Kirsch Claims 26x VAERS Underreporting Factor, Challenging Official Vaccine Safety Data Interpretation
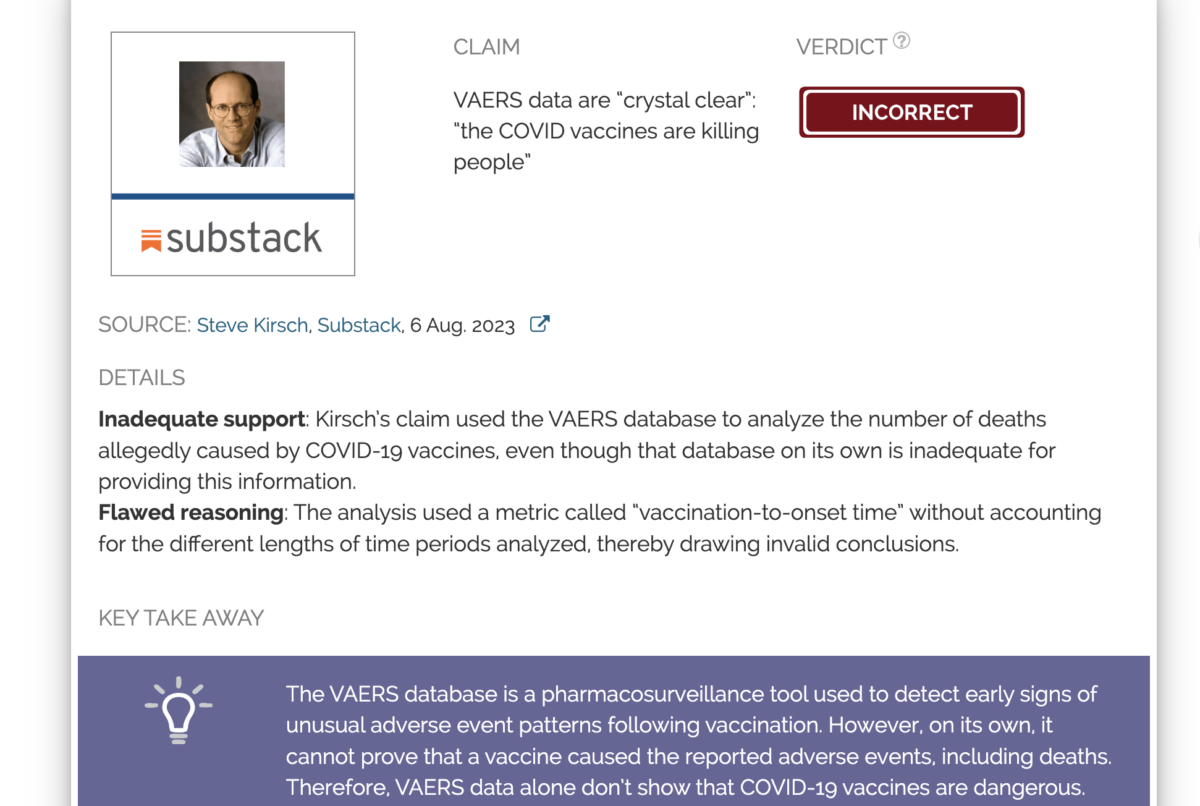
Steve Kirsch, a prominent figure known for his skepticism regarding vaccine safety, recently asserted that the Vaccine Adverse Event Reporting System (VAERS) operates with an underreporting factor (URF) of "26x or higher." This claim, disseminated via social media, suggests that the actual number of adverse events following vaccination is substantially greater than officially recorded in the U.S. government's surveillance system.
VAERS, jointly managed by the Centers for Disease Control and Prevention (CDC) and the U.S. Food and Drug Administration (FDA), functions as a passive surveillance system. Its primary role is to detect potential safety signals that warrant further investigation, rather than to establish causal links between vaccines and adverse events or to determine incidence rates. The system explicitly states that reports are voluntary and vary in quality, and that the number of reports alone cannot be used to draw conclusions about the frequency or severity of problems.
Kirsch's assertion of a 26x or higher underreporting factor implies that for every one adverse event reported to VAERS, 25 or more go unreported. Proponents of such high multipliers often derive them by comparing VAERS reports to expected adverse event rates from clinical trials or other data sources. This methodology leads to significantly inflated estimates of vaccine-related injuries and deaths.
However, health authorities and independent experts largely dispute the application of a single, high underreporting factor to all VAERS data, especially for serious events. While underreporting is an acknowledged limitation of passive systems like VAERS, its degree varies widely depending on the type and severity of the event. For minor reactions like soreness, underreporting is high, but for serious events, reporting rates are considerably higher, with some studies indicating that a large percentage of suspected serious events are reported.
The context of COVID-19 vaccine reporting also introduced unique factors. Healthcare providers were, for a period, required to report all deaths following COVID-19 vaccination, regardless of suspected causality, a mandate not consistently applied to other vaccines. This difference can lead to a higher volume of reports for COVID-19 vaccines in VAERS, which does not equate to a higher incidence of vaccine-caused events. Studies have also suggested that political inclination may influence the motivation to report adverse events, further complicating direct interpretation of raw VAERS data for incidence.
The CDC and FDA consistently emphasize that VAERS data serve as a hypothesis-generating tool, prompting further investigation through more robust epidemiological studies. They caution against misinterpreting raw VAERS data to infer causation or to calculate actual rates of adverse events, reinforcing that a report to VAERS does not prove a vaccine caused the event, only that it occurred after vaccination.